Greetings and welcome to Inside Venture7! In this session, we will delve into a crucial aspect of customer service that affects everyone at some point: healthcare. Today we have with us Mr Narender Kumar, CEO of Venture7.
We will talk about recent changes in Star rating criteria by the Centers for Medicare & Medicaid Services (CMS). How does attrition in the payer call center impacts customer experience?
Let’s kickstart our conversation.
Team Venture7: What change did the Centers for Medicare & Medicaid Services (CMS) bring in the methodology for calculating Medicare Advantage (MA)?
According to the contract year 2021 Medicare Advantage and PartD Final Rule (CMS-4190-F1), May 22, 2020, changed the methodology for calculating Medicare Advantage (MA) quality scores. The change is that customer-experience-related metrics would determine 57% of overall Stars ratings (up 25 percentage points) by 2023.
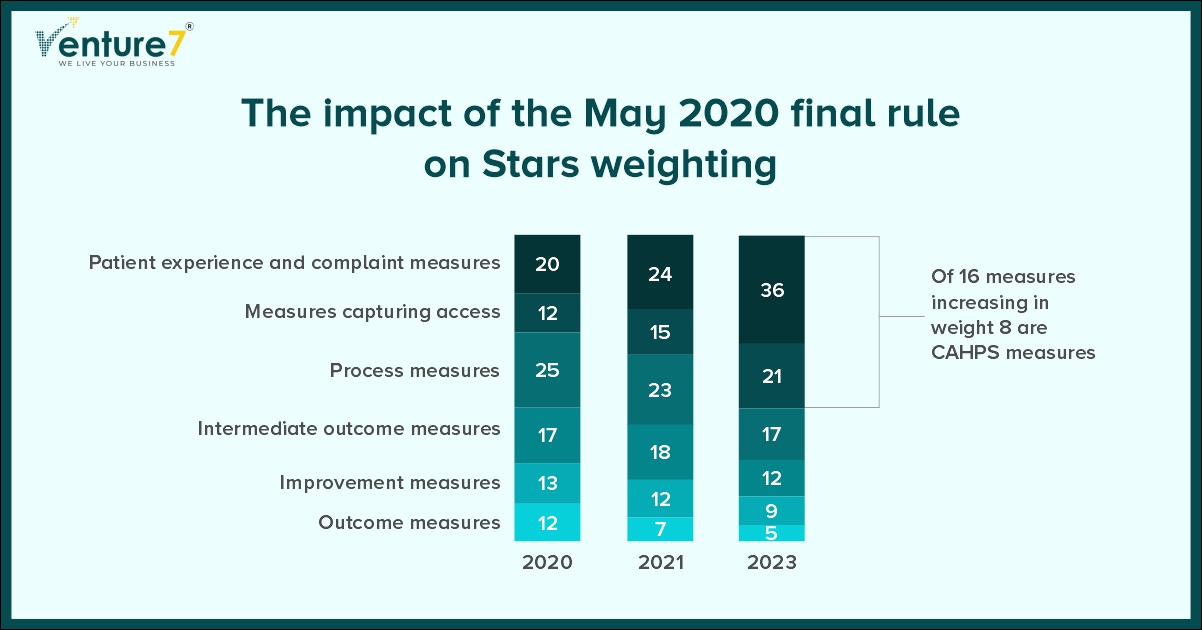
Team Venture7: How does a Star rating impact?
Improving star ratings not only prioritizes health plan quality but also introduces payment incentives by the government to MA payers for enhancing the quality of patient care.
According to research findings, obtaining an additional 1-Star rating can lead to an 8% to 12% surge in MA enrollments. Similarly, if the rating improves by 3 to 4 Stars, there can be a revenue boost of 13.4% to 17.6% in the subsequent year.
Team Venture7: What is your perception regarding the growth of the Medicare market?
As of 2030, every baby boomer in the United States will have reached the age of 65, which means they will be qualified for Medicare. According to the U.S. Census Bureau’s projections, this accounts for approximately 20% of the population.
According to the Kaiser Family Foundation’s 2021 report, more than 3,500 Medicare Advantage (MA) plans were offered to eligible beneficiaries. Out of the 63 million seniors eligible for Medicare, over 26 million, more than 40%, have enrolled in MA plans.
The market is expanding, and so is the competition.
Team Venture7: In healthcare payer contract centers, how does customer service representative attrition affect customer experience-related metrics?
It affects negatively.
Continuous recruiting, hiring, and onboarding processing can cost up to nine months of a CSR’s salary. Additionally, it can take six to nine months to train a new CSR.
If a payer is experiencing high attrition, it will add to a huge cost.
I will like to pinpoint here what is high attrition level. A high attrition level is 25% ++.
Many payer contact centers are experiencing 30% attrition.
Team Venture7: Can you provide insights on the reasons for high attrition rates in healthcare payer contact centers?
One major reason why customer service representatives have a high turnover rate is due to a work-related syndrome called “burnout” caused by stress. CSRs may display burnout symptoms such as arriving late to work, leaving early, lacking motivation, and eventually quitting. Most CSRs deal with repetitive tasks that are both time-consuming and prone to errors. The nature of the job can be demanding, and a lack of management support and recognition can add to the pressure.
Benefit inquiries are the most common reason for calls to Payer Call Centers. Our experience working with various Health Plans has shown us the common challenges they face when handling these inquiries are:
CSRs struggle with outdated systems and multiple sources when searching for benefits information. This can lead to a tedious process of up to 12+ steps and clicking through 7-11 systems.
Did you know that around 40% of the time is spent in silence during calls about benefits inquiries? This means members are kept on hold while customer service representatives search for relevant information.
It has been observed that approximately 25% of benefit inquiry calls need to be followed up with a call back to customers, especially for more complicated inquiries.
This situation not only causes stress in the workplace, resulting in high CSR turnover rates, but it also leads to a poor customer experience, which affects call center performance and hurts the Payer’s business.
Which ultimately results in:
- Low first-call resolution rates
- Increased call handle times
- Low KPI achievement
- Frustration for members and providers
- Reduced Star ratings and NPS
Digital transformation can help resolve this impasse. The solution should be such that it helps the human agent to find the accurate and latest information fast. It should help the agent to become more productive.
Treating your team with the same care and attention you would give your patients pays dividends in the long run. They’ll be more committed and likely to leave positive reviews on sites like Glassdoor if they ever leave. Negative comments like “Avoid this employer like the plague” will be avoided altogether.
Investing in making their task easier and faster propels higher satisfaction.
Team Venture7: As we end our conversation, I would like to know your views on the potential impact of AI on customer service and support in healthcare. What changes do you think we can expect in this area?
You may have encountered this study, which suggested that AI provided more empathetic responses to patients than real-life interactions.
It’s quite alarming because they begin with, “Oh, hi. I’m sorry you’re not feeling well.” How often does your healthcare provider say that? They immediately show empathy, not just rushing to business. Taking that energy and expressing genuine concern can be a powerful tool. For those who struggle with empathy, AI could become an invaluable resource to develop this skill. It’s intriguing to see where AI will lead us in enhancing bedside manners and empathy in healthcare.
However, we will like to prioritize the application of AI that makes the research of customer service representatives faster and easier.
We had a wonderful time. At some point in the future, we can talk about how AI can enhance productivity and reduce stress for service agents.